Medicare released extensive data last week about how much it paid to providers in 2011. The data set includes information about various procedures and how expensive they were, who performed them, how many they performed, the average cost of each procedure and the average reimbursement provided by Medicare.
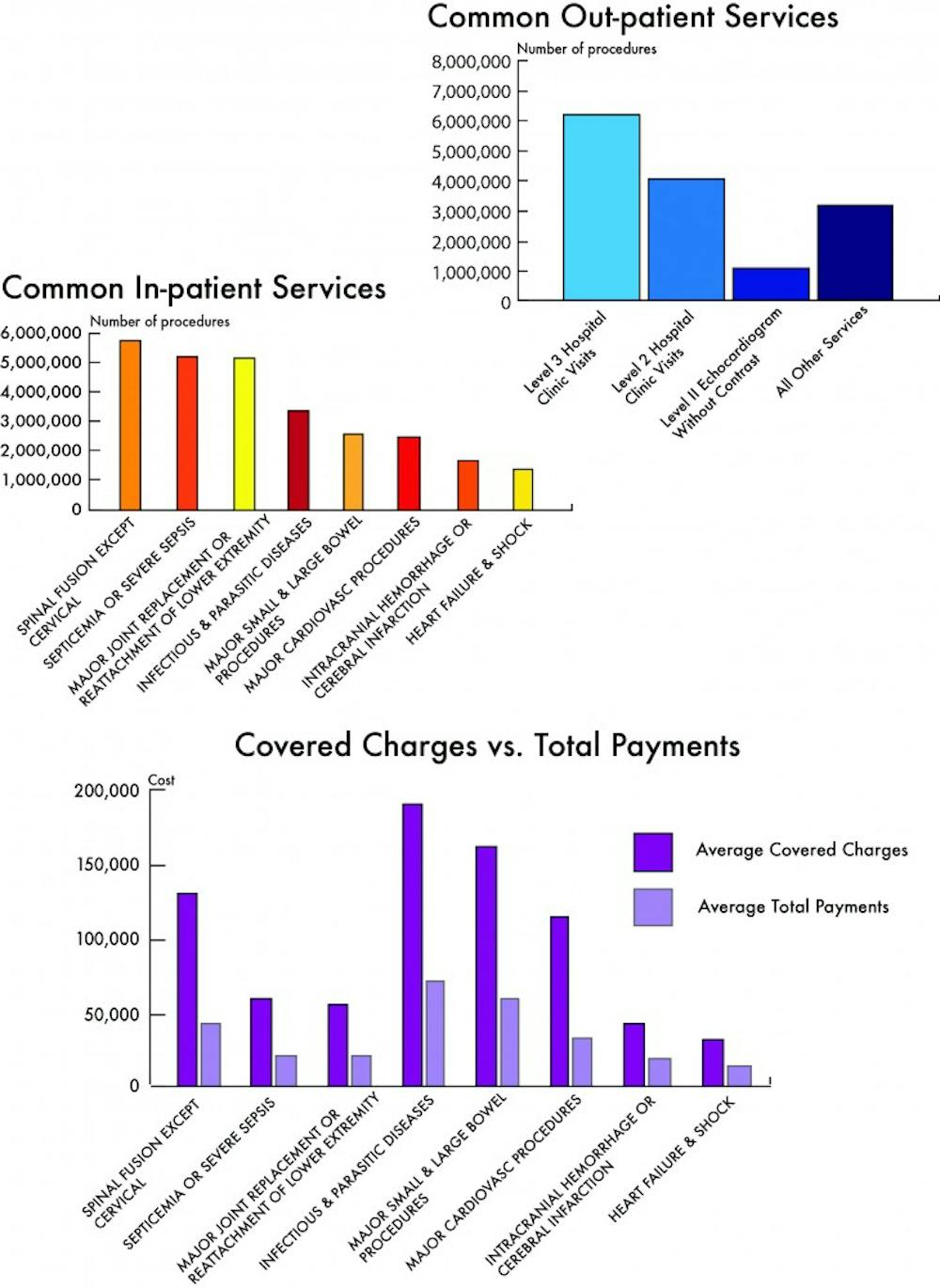
The data release included information on the University Medical Center and its Medicare related procedures. For the 28 outpatient procedures listed, Medicare paid a total of $14,600,718.49 to the Medical Center and, for the 91 inpatient procedures listed, Medicare paid a total of $76,850,532 to the Medical Center and Health Sciences Center.
Notably, there was a sizeable disparity between how much providers, such as the Medical Center and its doctors, charged Medicare and the actual amount Medicare paid them. Overall the University’s claims, or the amount it charged Medicare, for outpatient services totaled $37,070,125.36 and the claims for inpatient services totaled $210,742,860. In the case of outpatient procedures, most of the claims came from clinical visits to the Medical Center.
“This is common for hospitals and all other providers across the U.S., as Medicare payments are set by law and are typically well below hospitals’ prices,” Swensen said in an email.
The amount Medicare pays for certain coded procedures depends on well-established policy based on the nature of the procedure.
Medical School Prof. Carolyn Engelhard, a fellow at the Batten School Center for Health Policy, said people will be able to use this information to make important decisions about health care going forward.
“It will be used to look at appropriate utilization of Medicare services,” Engelhard said. “Up to 30 percent of everything [providers] do is probably wasted.”
Engelhard said this specific data shows information on what procedures providers are performing and how often they are performing those procedures. Patients should be able to use this information as a tool when choosing a health care provider.
“There are more Internet tools that consumers are using to look at [health care data],” Engelhard said.
Engelhard said a Medicare patient who is unsure about whether or not to undergo a procedure can look at the amount of times a provider has performed it and go from there.
“You might go to this dataset to see if [a] physician does a ton of other procedures,” Engelhard said.
Engelhard said the government could use this data as well, since it could serve as a tool to detect health care fraud.
“People could use it to weed out abuse in the system,” Engelhard said. “I think that is the hope behind it.”
People still need to take this approach to the data with caution, Engelhard said, because the data only shows the volume of procedures, not their outcomes, and there can be many reasons why there is high volume for certain procedures.
“This just looks at volume,” Engelhard said. “It doesn’t really tell us whether the care was delivered in an effective and cost-effective way.”
The University launched an Accountable Care Organization in January for some of its Medicare patients. The ACO saves money when patients cost less to treat, so the Medical Center can make money by improving health care quality and decreasing the number of procedures it gives patients.
An article in JAMA Internal Medicine from last year found many echocardiograms, a specific type of diagnostic test for heart problems, did not cause doctors to change the kind of care they were giving. The authors said their results indicated echocardiograms were potentially being overused.
Medicare paid the Medical Center $1.17 million for echocardiograms in 2011, making the diagnostic test the second largest outpatient charge for the Medical Center. Swensen said the Medical Center only looked to give patients the best care possible.
“We always seek to make decision on tests, imaging and procedures that are in the best interest of our patients and to provide the best possible care,” Swensen said.
The University received $5.7 million from Medicare for performing spinal fusion surgery and $5.1 million for performing major joint replacement surgeries, such as knee and hip replacements. Both spinal fusions and joint replacements are often elective, rather than done in an emergency.
Swensen said, regardless of the Medicare data release, the Medical Center’s first priority is to develop means through which to best care for its patients.
“In this rapidly changing health care environment, we will continue to focus in the future on ensuring we are providing the right care at the right time and in the right place for our patients,” Swensen said.
Engelhard said this data release may prove useful, but ultimately it cannot stand on its own.
“Any data like this has to be taken with a grain of salt,” Engelhard said.