Daniel Gioeli, an associate professor in the University’s Department of Microbiology, Immunology and Cancer Biology, has worked with a Charlottesville-based biotechnology company to successfully recreate a cancer tumor environment outside of a patient’s body.
The company, HemoShear Therapeutics, was founded by two former University faculty members in 2008. Brian Wamhoff, the head of innovation at HemoShear Therapeutics, said the company is focused on developing therapies for rare diseases, primarily in the liver, called inborn errors of metabolism.
According to Wamhoff, the process of creating a 3D tumor model started when the National Cancer Institute noticed HemoShear Therapeutics’ work on recreating liver diseases outside of a patient using their diseased tissue. The NCI believed that these principles could be applied to cancer research and issued a NCI Small Business Innovation Institute grant of $2 million dollars to HemoShear Therapeutics to develop a platform to discover new therapies for cancers.
Upon receiving the funding, HemoShear Therapeutics evolved the current technology and experimental methods they used to study these rare liver diseases to research cancers that have high mortality rates but few treatments, such as pancreatic cancer and lung carcinoma.
During this process, the company also realized they needed the expertise of a cancer cell biologist. They approached Gioeli in 2016, who was at the time on sabbatical from the University to work with HemoShear Therapeutics as Senior Director of cancer biology.
Gioeli, in collaboration with HemoShear Therapeutics, set on a mission to recreate patient tumors outside of the patients.
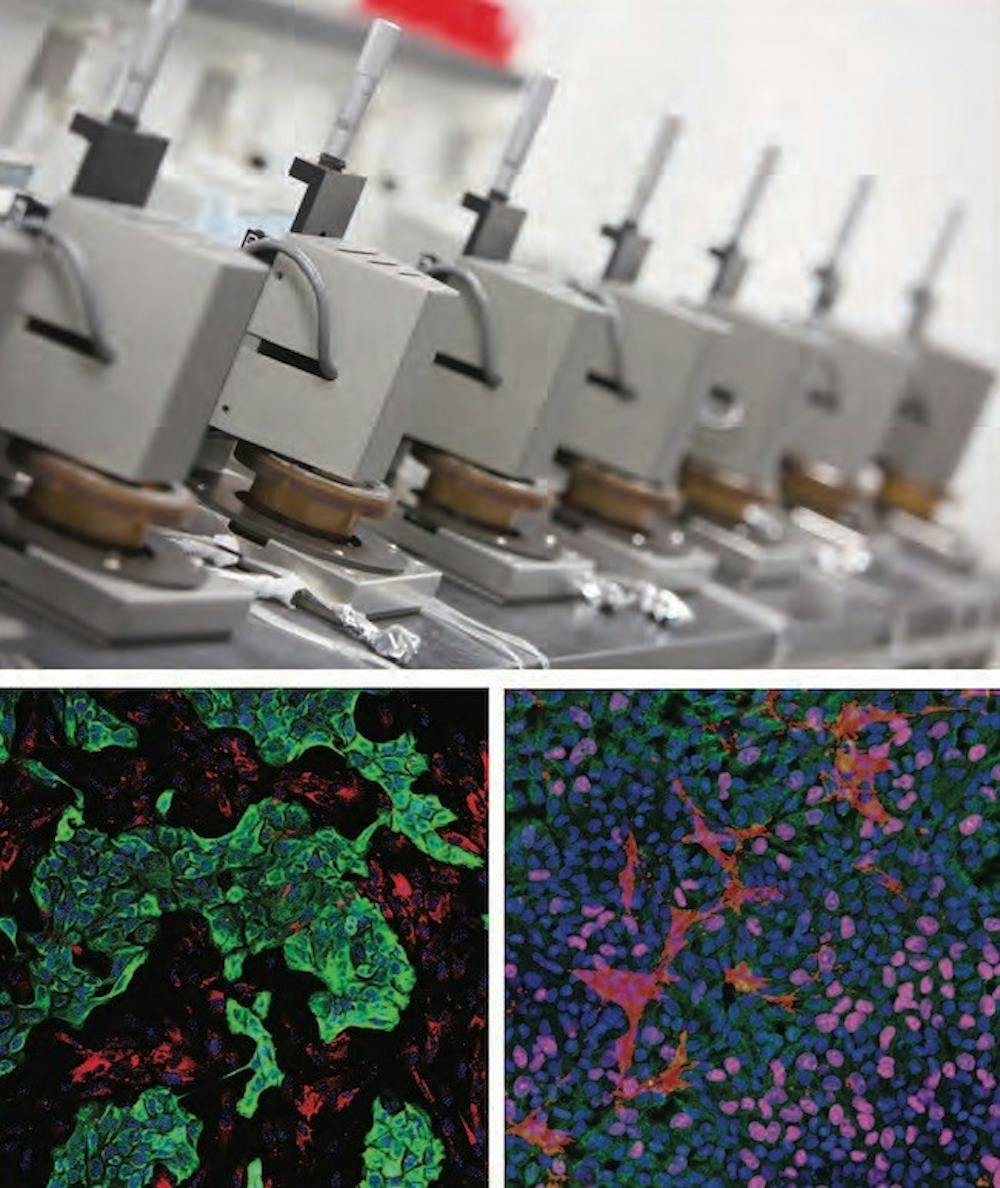
Wamhoff said a tumor cannot be recreated by simply transferring tumor cells from a patient to a petri dish. This is because the environment of the tumor in the body is different than just a single, isolated tissue culture in a petri dish. Thus, HemoShear Therapeutics focused on recreating the environment of the tumor in the 3D model.
“Think of it as a three dimensional recapitulation of the patient’s tumor that includes blood flow and all of the cell types necessary for the tumor to grow in a human outside of the patient,” Wamhoff said. “It’s like creating an avatar of the patient’s tumor outside of them to study it and then figure out what drugs could impact that tumor and then go back to the patient with that therapy.”
According to Gioeli, a large amount of time was spent optimizing the 3D model using both existing and new knowledge. Gioeli and HemoShear Therapeutics had to combine what they already knew about how blood vessel cells respond to mechanical forces with new information on how tumor cells and stromal cells — normal body cells that get corrupted by tumor cells — interact in a model with vascular endothelial cells, the cells that line blood vessels.
Wamhoff said one of the biggest challenges with treating cancer, especially for Stage IV patients, is finding the right treatment in a limited amount of time. A patient’s tumor can be introduced into this 3D model and customized to test the effectiveness of different drugs on the particular patient. This model would enable users to find medications that patients may have a better chance of responding to prior to starting actual treatment.
Gioeli and his team presented this new model in Boston at the 3D Tissue Models Oncology 2018 meeting. He said the response from other academics was positive and various discussions took place surrounding this model.
Unlike previously created models, this model uniquely incorporates different cell types such as vascular endothelial cells. Since tumor cells interact with several different cell types to function in the human body, adding different cell types to the petri dish helps the replicated tumor better simulate the tumor in the patient.
“Not many models incorporate that and no model does it the way we do,” Gioeli said.
According to Gioeli, the empirical data obtained in the lab has shown that the biochemistry of the tumor cells in the model correlate well with those of the actual patient. The response of the tumors to the drugs also parallel the clinical responses seen in the actual patients.
Another method to study a patient’s tumor is by injecting their tumor cells into a mouse, which then starts to grow the human tumor. Different drugs can then be tested on the mouse to study the responses.
Wamhoff said that the data gathered from research shows early indications that their 3D system is proving to be better than the mouse model, which is currently the gold standard in the cancer therapeutic industry. This is because their model appears to be more “human” than existing ones, meaning the way the model responds to drugs and other stimuli closely aligns with how humans respond.
Moving forward, Gioeli and HemoShear Therapeutics hope to utilize this model in fundamental drug discovery to evaluate and even discover new therapeutic targets in cancer. They also want to develop a patient avatar — a digital representation of the patient that simulates key medical components — to predict responses to different drug treatments and create an individual test for personalized medicine.