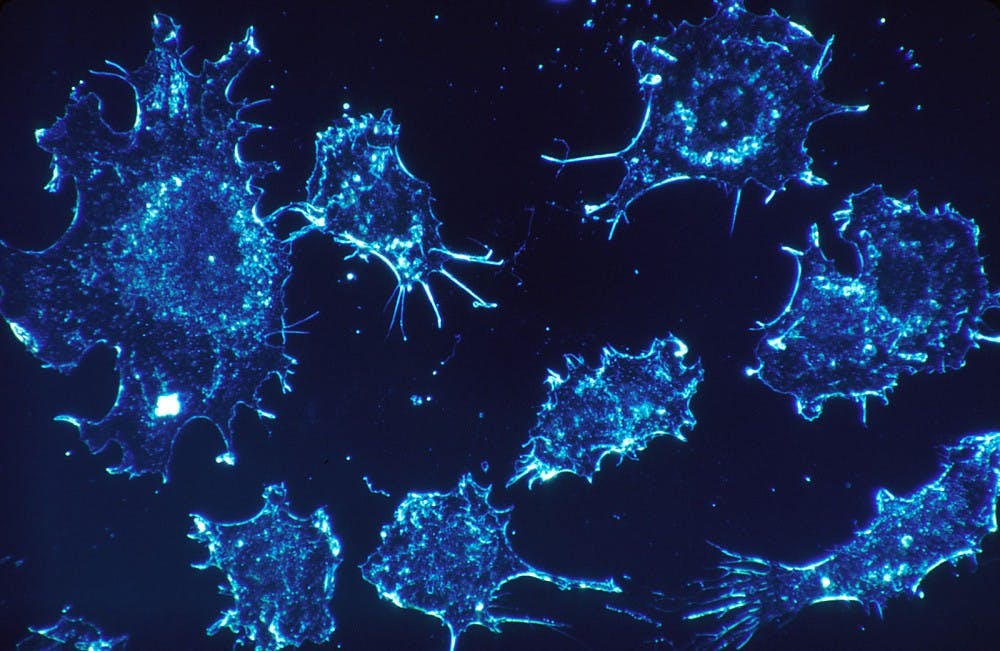
Repairing damaged tissue is a process the body automatically undergoes as needed. However, new research from the Dudley Lab in the University’s Department of Microbiology, Immunology and Cancer Biology demonstrates that what is usually helpful may also be a means by which harmful tumors survive and spread.
Doctorate student James V. McCann, the researcher who spearheaded this particular project, began investigating the ways in which tumors subvert the wound healing process approximately four and a half years ago in the Dudley Lab. Led by Andrew Dudley, associate microbiology, immunology and cancer biology professor, the lab seeks to understand blood vessel production in cancerous cells and the impacts the tumors’ microenvironment, or immediate surroundings, have on their maturation and metastasis.
“The overarching goal in the lab is to understand how different types of cells in the tumor microenvironment affect the growth of the tumor,” McCann said. “If we can understand certain pathways that these cells exploit or co-opt, then we can try to understand their biological function and ultimately try to design therapies based on these insights.”
Specifically, McCann examined the aspects of tumors that are analogous to wounds that persist indefinitely, such as their habit of directing disproportionately large amounts of blood to themselves. A steady blood supply is critical to cell survival, cancerous or otherwise, as blood acts as a delivery system for oxygen and vital nutrients. Tumors recruit blood vessels at a rapid rate. As a result, they can grow and disseminate in an uncontrolled fashion.
“For a while, it’s been recognized that tumors are like un-healing wounds,” McCann said. “They are known to subvert or exploit normal processes for their own growth and development.”
Multiple research methods aided in uncovering this unique approach to controlling tumor expansion. Since tumors vary based on their initial growth site, McCann focused his initial research on breast and lung tumors, two representative subsets of cancer often studied in the Dudley Lab. He compared cells from diseased and healthy mammary or lung tissues, both in culture — outside of an organism — and in living hosts, namely mice. Detailed scrutiny of endothelial cells, or cells within blood vessels, and the blood vessel development pathways highlighted discrepancies amongst individuals cells in both types of tissue.
What McCann and his colleagues found was that the endothelial cells differ with respect to their affinity for the presence of fibrin, a protein that plays a critical role in staunching blood flow from injured blood vessels and in promoting blood vessel formation.
Furthermore, the determination of the cells’ reaction to fibrin relies on molecules known as microRNAs, which help manage gene expression. Data from McCann’s study indicated that greater concentrations of these microRNAs in the endothelial cells decreased fibrin accumulation, thereby impeding blood vessel establishment.
During the normal wound healing process, the body coordinates the number of endothelial cells that facilitate fibrin deposition and degrade it. Tumors then abuse the body’s balancing act between endothelial cells that facilitate fibrin deposition and those that degrade it. McCann shared his hope that these novel insights may provide a solution to tumor regulation.
“If you can manipulate this pathway, you can inhibit blood vessel density or the number of blood vessels in the tumor, and that affects its overall growth and development,” McCann said. “That was the overarching goal, to understand what is different between tumor blood vessels and normal ones, what is the genetic signature that is potentially responsible for that and if we manipulate it, what happens to the growth and development of the tumor.”
Dudley offered his support for all that McCann has done, not only through guidance in the lab but also in his insistence that McCann be recognized.
“I want to give James full credit,” Dudley said. “He was the one who really took the initiative for this project, and he did an outstanding job moving the research forward.”
Implementing the knowledge gained from years of experimentation is the next step. Before translating conclusions to the everyday treatment of cancer — a journey that could be years in the making — McCann identified the need to analyze whether or not they could be extrapolated to other forms of and metastatic cancer.
While all tumors do not behave exactly alike, as their microenvironment can dictate many of their characteristics, a commonality is their tendency to cause blood vessels to leak. Subsequently, cancer cells promote fibrin generation, leading to the creation of blood vessels and augmented access to a blood supply.
“We looked specifically in mammary tumors and lung tumors, but one thing that is known about a lot of tumors is that the blood vessels are leaky, which leads to the deposition of fibrin in a wound healing-like response,” McCann said. “We think that this process is probably active in multiple types of tumors. We are in the process of testing that right now.”
McCann also mentioned more avenues for exploration. For instance, blood vessels do not operate in isolation but rather in concert with immune cells. The communication that occurs between them may help craft a more complete profile of cancer progression.
As research continues, an intermediate milestone on the way to witnessing implications for cancer treatment in human patients might be repurposing available drugs that influence the wound healing process. Though the Dudley Lab will not necessarily be the ones to undertake the task, McCann cited this as a logical next step, and emphasized that, above all, the intention is to improve human health.
The National Institutes of Health, the American Cancer Society, an AACR-Bayer Innovation and Discovery Grant and the U.S. Army Medical Research and Materiel Command’s Armed Forces Institute of Regenerative Medicine funded McCann’s research in the Dudley Lab. A paper detailing the research was published in the April 2019 issue of The Journal of Clinical Investigation.