Researchers collaborated across the University’s School of Medicine and the School of Engineering and Applied Science to develop a new 3D bioprinting method known as DASP — Digital Assembly of Spherical Viscoelastic Bio-Ink Particles. DASP will offer greater structural versatility and better mimics the body’s natural conditions compared to current bioprinting techniques — the group is currently working together to apply DASP to type 1 diabetes transplant mechanisms.
DASP offers beneficial modifications for a variety of other biosynthetic applications as well. Through 3D bioprinting — a versatile tissue engineering technique — researchers can create cells, important molecules and artificial tissue that closely resembles human tissue and organs. Applications range from studying drug effectiveness to medical modeling to organ transplants.
Liheng Cai, assistant professor of biomedical engineering, leads the team.
“When you think about 3D bioprinting, it offers a very good control on creating complex architectures, which mimic the geometry and biological functions of tissues and organs,” Cai said. “This is really the hope — and also the promise — that 3D bioprinting poses.”
However, the standard bioprinting techniques have functional limitations. Bioprinting currently mixes hydrogels and cells to produce bio-ink filaments. Hydrogels are 3D networks of hydrophilic polymers that can swell in water and simultaneously retain both the water and their structure. The filaments are stacked layer by layer to construct 3D structures, which does not very accurately mimic the body’s natural environment and has more structural restrictions.
“You [build] layer by layer to create a 3D structure … but this does not really reproduce what nature does,” Cai said. “In real biological tissues, each cell is surrounded by many other cell types, and also surrounded by many other proteins.”
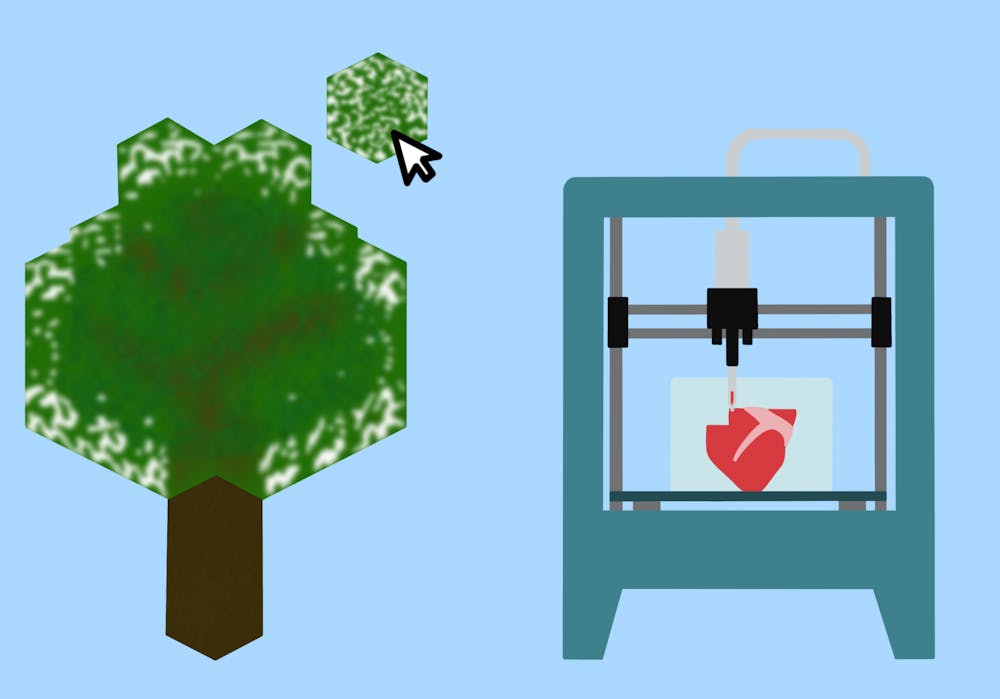
While considering how to remedy this problem and expand the capability of bioprinting, the engineers drew their inspiration from the video game Minecraft. Minecraft utilizes voxels, which are small cubes to build objects in a universe of the player’s creation.
“In there, using those kinds of voxels, it’s like small cubes of different colors and flavors to create various kinds of cartoons of even objects,” Cai said.
While video game players can create diverse characters and objects from these digital voxels, the engineers considered how to create cellular structures and tissues from biosynthetic voxels. Since players can construct buildings, characters and other objects from singular voxels of many different materials — such as red sandstone and polished diorite — applying this concept to creating biosynthetic materials from individual droplets addresses those functional limitations.
“That’s really our long term goal — to create a biological voxel to assemble those voxels into 3D tissue mimics,” Cai said.
The team ran into two main challenges in developing a biosynthetic voxel. The biological materials used to create voxels are very viscous, making it difficult to detach the printer nozzle from these droplets, which affects the precision of their shape and placement. The second challenge was finding a way to fix these droplets in a space before assembling the droplets together.
According to Jinchang Zhu, lead author and doctoral student in Cai’s laboratory, it requires great precision.
“3D printing is about putting the right cell in the right place,” Zhu said.
To work around the first challenge, the team engineered a reversible process where the 3D printer nozzle releases individual droplets in a supporting matrix, rather than in air, so that the nozzle can be detached more easily and droplets can be precisely placed. In its water-soluble environment, these droplets — or voxels — swell and partially merge together after being placed in the supporting matrix, forming a complete structure made of distinct droplets.
“So think about a gummy bear, right?” Cai said. “If you throw a gummy bear in the water, the gummy bear will swell.”
Similarly, the swelling creates a 3D structure made of distinct voxels that are much smaller than filaments and therefore offer more structural versatility. Additionally, they better mimic real biological tissues composed of distinct, individual cells, rather than filament layers.
The team, working alongside their doctoral student Yi He, found a specific application for DASP in collaboration with Assoc. Prof. Yong Wang from the School of Medicine and Jose Oberholze, professor of surgery and biomedical engineering and director of the Charles O. Strickler Transplant Center, who are working on improving type 1 diabetes transplants. Type 1 diabetes is a chronic condition afflicting 9.5 percent of the global population where the immune system falsely perceives islet beta cells as foreign invaders and destroys them.
These cells — located in the pancreas — are responsible for producing insulin, which is necessary for the body to intake sugar and produce energy. Patients have to take in insulin in order to make up for this deficiency, but transplanting the affected cells is a common way to allow patients to make up for their damaged cells.
The new islet transplants are not entirely resilient. Conventionally, millions of individual cells are encapsulated in microcapsules and transplanted, spreading and aggregating over time until the cells can no longer properly sense glucose. It is also difficult to retrieve these transplants once they begin to fail or if something unexpected occurs.
“For any device you put in a human body … you always want to retrieve it whenever you want, just in case something bad [happens],” Zhu said. “However, because these droplets are really tiny and individual, they’re … basically everywhere. It is almost [impossible] to take them back.”
DASP could potentially solve these issues by printing these individual cells directly into a 3D structure for transplantation, rather than transplanting individual cells that can travel, sink and aggregate together, as Wang said.
“If [you] define the 3D structure, maybe they can sense the glucose much better and much more favorably,” Wang said.
DASP’s scaffold is currently designed to be a temporary structure with the goal of training cells to form tissue structure. However, islet transplants would require structural support, so the supporting matrix has to be strengthened in order to stay in a diabetes patient’s body long-term to offer functional cells. Currently, the DASP technique is being tested in mice, and the researchers will continue observing the effects of the transplants. If successful, the researchers will proceed with clinical testing in non-human primates.
Since DASP generally offers more structural flexibility and precision in its novel approach, the researchers expect that they may have other applications. For example, DASP can be used to study different types of cells in different droplets or voxels.
“You can monitor and observe the interaction between these three kinds of cells, like to create a tissue model,” Zhu said. “This tissue model can really be helpful for some disease model or drug screening.”
In the meantime, the interdisciplinary team continues to work together on their specific niche in bioprinting, adapting their Minecraft-inspired technique, DASP, to islet transplants and looking toward the next steps.
“That’s really [the advantage] here,” Cai said. “We can synergize fundamental research and the clinical cultures in very small segments.”