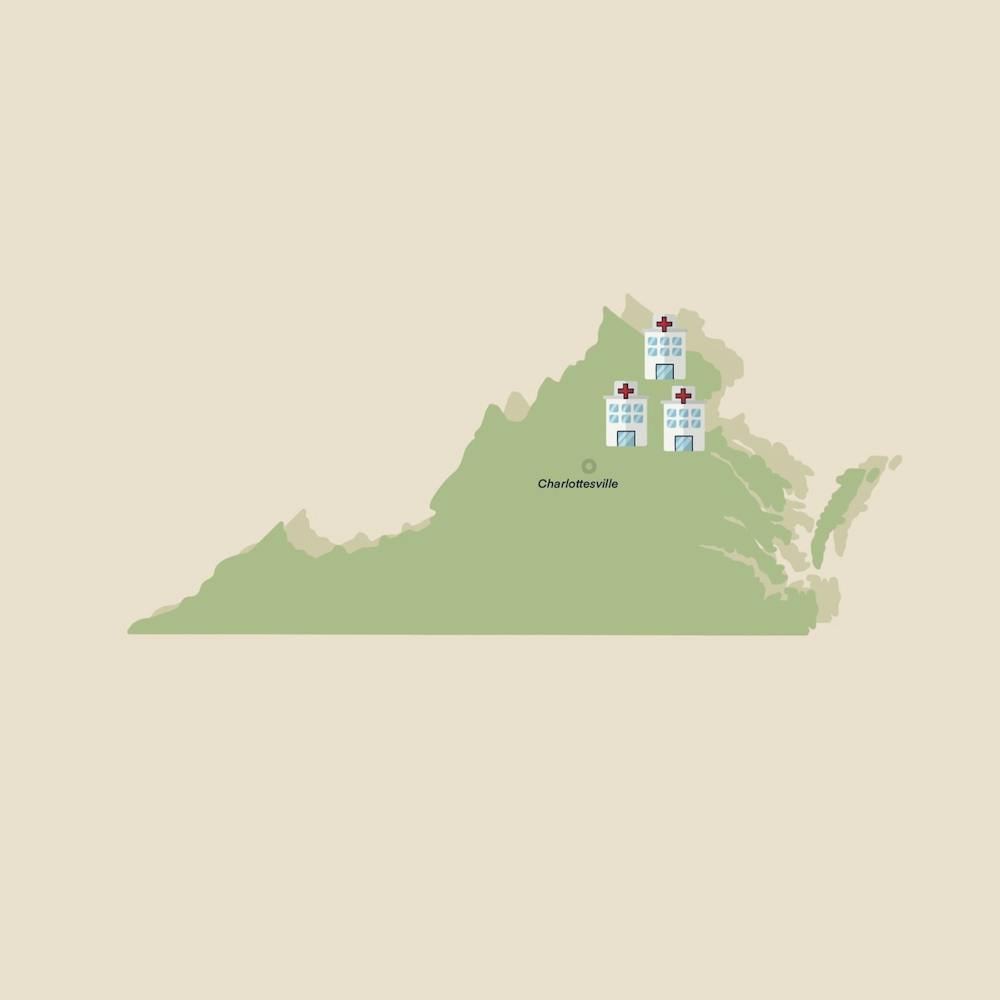
As of July 1, the University became the sole owner of Novant Health U.Va. Health System, a Northern Virginia regional health system previously owned by Novant Health and the University through a joint operating company. The University’s ownership now includes all the facilities and assets that were formerly a part of the joint-operating company, including Culpeper Medical Center, Haymarket Medical Center and Prince William Medical Center, among others.
For years, the nation’s shift towards building large consolidated hospitals has created a surge of debates regarding whether the trend would benefit patients or simply act as a business tactic under the name of expanding services. Many are concerned about compromising the decades-long relationships of regional hospitals and local communities as the market pressures independent operations to merge with rising consolidations.
Craig Kent, chief executive officer of U.Va. Health and executive vice president of health affairs, said the University plans to preserve the well-established relationship between community hospitals and local residents while adding a substantial boost to the hospitals’ current services.
“It's taking community hospitals but making them stronger, better, in terms of the care level they can provide,” Kent said. “But at the end of the day, we don't want to take away the essence of a community hospital.”
According to Kent, the three community hospitals already have exceptional primary and secondary care, which satisfies the needs for patients with less complex illnesses. However, the capacity of those hospitals is limited in providing tertiary and quaternary care, which require highly specialized equipment and expertise. As a result, patients with complex diseases have to drive long hours to receive necessary treatment. The University’s ownership will allow it to expand the scope of services patients in Culpeper and Northern Virginia can receive and make advanced medical care more accessible.
“We will grow tertiary care by hiring more physicians that will practice in those communities and be there,” Kent said. “Many of the people from those communities have to drive to Charlottesville or they have to drive to Fairfax to get their tertiary care. Now they'll be able to stay locally because we'll have people in those communities to provide tertiary care.”
Hospital consolidation also often leads to increases in price — a recent study conducted by Yale economist Zach Cooper and others found that there is a 12 percent increase in prices at monopoly hospitals compared to those in markets with four or more rivals. The locations of merging hospitals also play a factor in the price increase. Cooper and his colleagues observed a price increase of over 6 percent when the merging hospitals were geographically closer — for example, 5 miles or less apart — but not when the hospitals were geographically distant.
In response to the inflation of healthcare costs, Kent explained that money can be, in a way, saved through consolidation of the healthcare system. By expanding the scope of care in Culpeper and Northern Virginia, disease prevention could be better achieved and the cost of going through advanced procedures could be avoided.
“Getting care locally when it’s needed in the end saves money for healthcare because we give care on a timely basis and it keeps diseases from advancing,” Kent said. “A great example of that is if you have enough primary care physicians and they do all of the preventative work ... [it] saves the healthcare system money and it keeps people alive longer.”
According to Kent, a lot needs to be done in order to meet the University’s mission of serving residents with outstanding patient care throughout the Commonwealth. Kent points out that one of the many aspects that could be improved is the medical record system, which is currently unsynchronized among the three community hospitals. Synchronizing medical records would assist the University’s hospitals in communicating with one another and allow seamless transfer of medical records when patients are transferred between hospitals.
A second area of improvement is offering greater access to care by growing the physician workforce. Kent points out that there are simply not enough primary care physicians to meet the healthcare demand. In addition, healthcare specialists who could provide tertiary care should also be sent to the three hospitals. Therefore, a lot of time is currently spent on recruiting more healthcare professionals in those hospitals.
“We have a long list of things,” Kent said. “A lot of work is involved and teams of people are coming together to figure out how to make those hospitals stronger, and better able to serve their community.”
The University has expressed a promising outlook on its goal of offering medical service to residents across Virginia, and time will tell if it’s able to meet those goals.